Last week’s online docuseries, ‘The Broken Brain’, looked at so many different aspects of brain health that I thought it would be a great theme to address here in my blog over the coming months.
Today’s focus is on depression. Not only do I see it a lot in clinic but also this is a condition that’s not gender or age specific. It’s global; it’s on the rise.

Some of the recommendations I’m sharing from ‘The Broken Brain’ may initially sound too difficult. Exercise can be a hard one for some when motivation is missing.
Or it may sound trite hearing “don’t eat processed, reduce sugar”. I agree, this isn’t new news, but the science behind it, which I’ll be sharing here, makes so much sense and can be empowering.
However deep you may be in your illness, here are some ideas and recommendations from the docuseries – gems of information to add to what you may or may not already be doing.
Depression can be such a complex, and sometimes seemingly impenetrable, health condition which is why the functional medicine approach works well. It looks at the whole picture rather than just the symptoms plus it can give more time to the patient, which is often lacking in conventional medicine.
Antidepressants or SSRIs may be valid short-term conventional remedies to get you through a period of depression due to, say, grieving or trauma or stress. They may end up being part of the prescriptive ‘whole’ treatment for someone, however, there can be side-effects to medications – an emotional blunting or a feeling of un-wellness as well as all the other mentioned side effects listed in the medication box!
(Saying that, if you are taking medication you must never stop cold turkey. Discuss any changes you’d like to make with your doctor or healthcare professional. Reductions should be made slowly, gradually, and with supervision).
Like most chronic health conditions, there are many different possible players with depression.
The first questions to answer may sound simplistic for a disorder that’s so multifaceted:
How did it all start? What else was going on at the time? You may not know yourself – what did indeed kick start it all!? It may feel like something you’ve lived with forever.
There are therapies that can help here – counselling or CBT or psychotherapy to name but a few. Search online, read about what is available in your area and seek support.
An action plan, however, that you can try for yourself could be to mentally page through your life’s events, writing a journal, putting down memories that come into your head. Doors can open up and let fresh air blow in, awakening thoughts which may help your process of understanding why you feel the way you do.
Possibly an ah-ha moment or two.
There are currently 3 epidemics that are affecting mental health – and overall health – in a big way.
1) Too much cortisol. This is an important stress hormone that works in tandem with adrenalin, another stress hormone; cortisol is supposed to ease off once the stressful situation – say, a tiger attack – is over.
I say tiger attack because this is how your body still functions. Nothing has changed much since early man’s days, so your body can’t differentiate between that tiger attack, or being stuck in traffic or running very late for an appointment. There’s no sliding scale, no ‘less’ pumping of stress hormones.
In our current society, cortisol levels often stay raised because the stress doesn’t stop, it just moves from one deadline to the next, from one traffic jam or ‘must do’ situation to the next. Finances, relationships, children, partners, jobs, school pick-ups, cooking meals…you name it, they are all potential and willing stressors in today’s fast paced world.
Even ‘playtime’ can be stressful (& is often self-imposed) with less outdoor sport or walks and social interaction, and more ‘online’ time, computer screens, social media time, mobile texting.
Stress is a big driver of depression. It cannot be underestimated.
Walking and even gentle movement if you find you can’t do more robust exercise, can relieve it by releasing endorphins, those happy neurotransmitters, especially if you combine it with scenery – the green outdoors, fresh air, parks, forests – and light.
Walking in sunshine ticks that other ‘outdoor’ box. Vitamin D, which is often low with depression, is made in your body and requires good cholesterol levels (cholesterol is not always the enemy!), and exposure to sunshine, at least 15 minutes on bare legs, arms, face…the more the better. Out of season, you could try using a lightbox.
Other de-stressors could be hobbies, movement classes (stretching, pilates, yoga) and mindfulness, a term we are hearing a lot at the moment – probably because it works!
There are currently so many mindfulness groups and sessions available around the country, around the world, so take a look at local noticeboards in your library, or ask in your local surgery or wellness centre.
For those who love ‘apps’, there is a plethora of relaxation apps – Insight Timer and Headspace to name just two. These can also help with sleep which is so essential for brain health. Even being deprived of sleep for only a couple of nights can heighten sensations of negativity and low mood!
2) Too much insulin.
Every time you eat something sweet, the hormone insulin is released from the pancreas to get the blood sugar back in balance, to move that sugar/energy to the body’s cells where the brain is assuming it must be needed (why else would this body have eaten so much glucose – must need energy to run away from that tiger, assumes the brain).
Think how many times a day you may be eating something sweet – from that white toast, to the pure orange juice (no fibre to slow down the sugar spike) and the biscuit or chocolate and evening glass of beer….
Insulin is being summoned by the brain again and again throughout your day – used and abused until your body becomes insulin resistant, unresponsive to the very hormone that is trying to keep blood sugar balanced.
This is our current diabetes, aka insulin epidemic. Worldwide.
Another fact about sugar is that it causes inflammation in the body plus, if inflammation is already going on – being overweight, ill from viral, bacterial infections, allergies, joint pain, migraines a.o. – it will just make things worse.
I’m referring to sugar in any form, not just the white stuff with your cuppa. Sugar in honey, maple syrup, alcohol, white bread (chew long enough and note how sweet those simple sugars in the bread taste) and fruit – but yes, fruit has fibre to slow down the sugar hit in the blood plus vitamins, phytonutrients, antioxidants – so a little is good.
And, most important, hidden sugars added to processed foods, often in the form of ‘ose’ names on labels (maltose, fructose, dextrose, lactose… loads of ose!)
Google all forms of sugar and be astounded.
Too many canned, bottled, packaged foods contain these ‘-ose’ sugars because your taste buds love them, they’re addictive, and so they sell and make money for the manufacturers at your health’s expense. Bluntly stated.
If you’re suffering from depression you may not like hearing that the very sweet food which feels like it’s lifting your mood is actually making your depression worse. The fact is, the lift is temporary. No sooner do you get that blood sugar spike, the brain will want to get it back to normal by calling in the insulin to drag it out of your blood – and you’ll experience a crash. That in turn will make you reach for yet more sugar.
Up and down, this seesaw can lead to insulin resistance and diabetes, weight gain and more depression.
Stopping sugar cold turkey is not the answer, but slowly reducing it might be. And what a great step forward – to help not just your mind, but to reduce the inflammation in your body and keep diabetes at a distance.
What can you eat instead? Fruit, as mentioned above, has many great nutrients, and will still help satisfy the sweet tooth to some extent. Best eaten in moderation – a couple of fruit a day such as a handful of berries, stewed apples or pears, some banana. Adding warm spices to stewed fruit such as cardamom or cinnamon will also help with blood sugar balancing.
And then an occasional sweet treat, a reward treat that you keep under control – as much as possible 🙂
Small steps are so effective – don’t beat yourself up if they don’t work all the time. Early days, one step at a time.
3) The third epidemic is not having enough thyroid hormone.
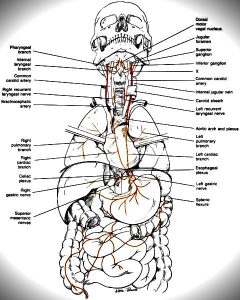
The endocrine – hormone – system is interconnected which means that the aforementioned adrenal stress can have a knock-on effect on your thyroid hormone.
Burning the candle at both ends for too long can result in adrenal fatigue and possibly hypothyroidism (you can also become hypothyroid via an auto immune route, but that’s another story for another day).
Your thyroid gland is responsible for your metabolism, for how efficiently you function, how energetic you feel, how fast your body digests and eliminates food and so on.
A healthy thyroid is about feeling sparkly rather than sluggish; feeling upbeat rather than low.
Its health will affect other hormones and neurotransmitters and has a direct impact on your nervous system health. Low thyroid – hypothyroidism – often has depression as one of its symptoms, so ask your doctor to check your thyroid levels because your depression may actually be a result of low thyroid function.
Drivers of inflammation that can lead to depression reel of the tongue easily:
Diet, stress, lack of exercise, toxins, infections….I’ve talked about some of these already.
Diet plays a huge role. Are you eating the necessary nutrients that will help make your hormones and neurotransmitters in order to keep your nervous system healthy and buoyant?
Good levels of protein – for cellular repair and feeling satiated – such as oily fish – ideal also for their brain-supportive DHA/EPA healthy fat levels – but also organic chicken, some organic or free-range meats, local lamb….
And if you’re vegetarian and don’t have intolerances or problems digesting pulses and eggs (choline in eggs, yes, another great brain food), do include these daily.
Go for smart carbs with low glycaemic load – all those rainbow vegetables which smack of vitality.
The more colour, the more phytonutrients they contain! These colours, just like the strong tastes or smells in certain foods (think of garlic, onion, cruciferous veg etc), equate to the plant’s effective defence system and dense phytonutrient content that will improve your own defences, your immune system and general wellbeing – and subsequently your state of mind.
The brain is the fattiest organ in your body. About 60% in fact. Therefore essential fatty acids, specifically omega 3s, are crucial for good brain function. Oily fish are the best source, but flaxseed, chia, all sorts of wild plants contain levels of omega 3s. (If you were going to supplement anything, it would be omega 3 fish oils that I’d be recommending first of all).
Consider, too, the healthy fats found in nuts and seeds, in avocados, olives and olive oil… And the saturated vegetable fat in coconut oil – how wonderful because saturated fats don’t oxidise in the brain the way unsaturated fats can be prone to free radical damage.
The next aspect to consider is, are you absorbing what you eat? I’ve seen more lab tests this year showing hidden infections and intestinal permeability than ever before. These will be compromising digestion & as a result will reduce absorption of the nutrients in your food.
If you have digestive symptoms – discomfort, reflux, flatulence, burping, pain – it would be invaluable to have a comprehensive stool test (sadly our NHS does not offer these tests) to ascertain if any hidden infections are in play.
Toxins! A huge topic, but briefly a lot of people can react negatively, with mood disorders, to toxic exposure such as chemical cleaning agents, fumes from carpets and paints a.o. Think about any toxic exposure you may have in the work place – chemicals? Mould in the building? Smokers around you?
Heavy metals is another blog in itself, but needless to say, this will be pulling down your immune system, and that in turn will affect your mind health. No myth that mercury caused the hatters of old to go mad. It is indeed toxic to the brain and can still be found in some amalgams, and certainly in some fish esp. large, old fish such as tuna, swordfish…
Finally and so importantly, exercise… or movement. Whatever you would like to call it! Whether it’s kickboxing or running or cycling or fast walking, rowing…..
There are so many options, you just need to find the one that appeals. Dancing may be your thing! All will be great for circulation, for bone health, for improving motivation and increasing those ‘happy’ hormones.
A last word about supplements.
There are a lot of supplements which you can read about online, and which are advertised to relieve your depression.
It is something to consider however start with the food you’re eating, the thoughts you’re thinking. Add a generous dash of daily movement, some kind and helpful support, tests from your doctor or private labs to rule out thyroid or gut issues….and take it from there.
You may find that swapping some foods, adding others, and going to a local zumba class gives you the uplifting start you need.
There are certainly wonderful herbs and complexes to suit all sorts of mood problems. All very individual, so it’s best to speak to a functional medicine therapist about it.
Make a start and then see where you want to go from there. Wishing you well on your journey!